Numa

Numa is a specialized procurement ecosystem designed to improve organ assessment and decision-making. It pairs an advanced imaging attachment with a collaborative mobile platform—empowering transplant teams to act faster, with greater clarity, and more confidence between provisional acceptance and surgery.
Project Lead, Product Designer
November 2024 – March 2025
Bryan Pek, Arden Hanks, Daniel Wong, Celine Pyun
Problem Definition
Our Solution

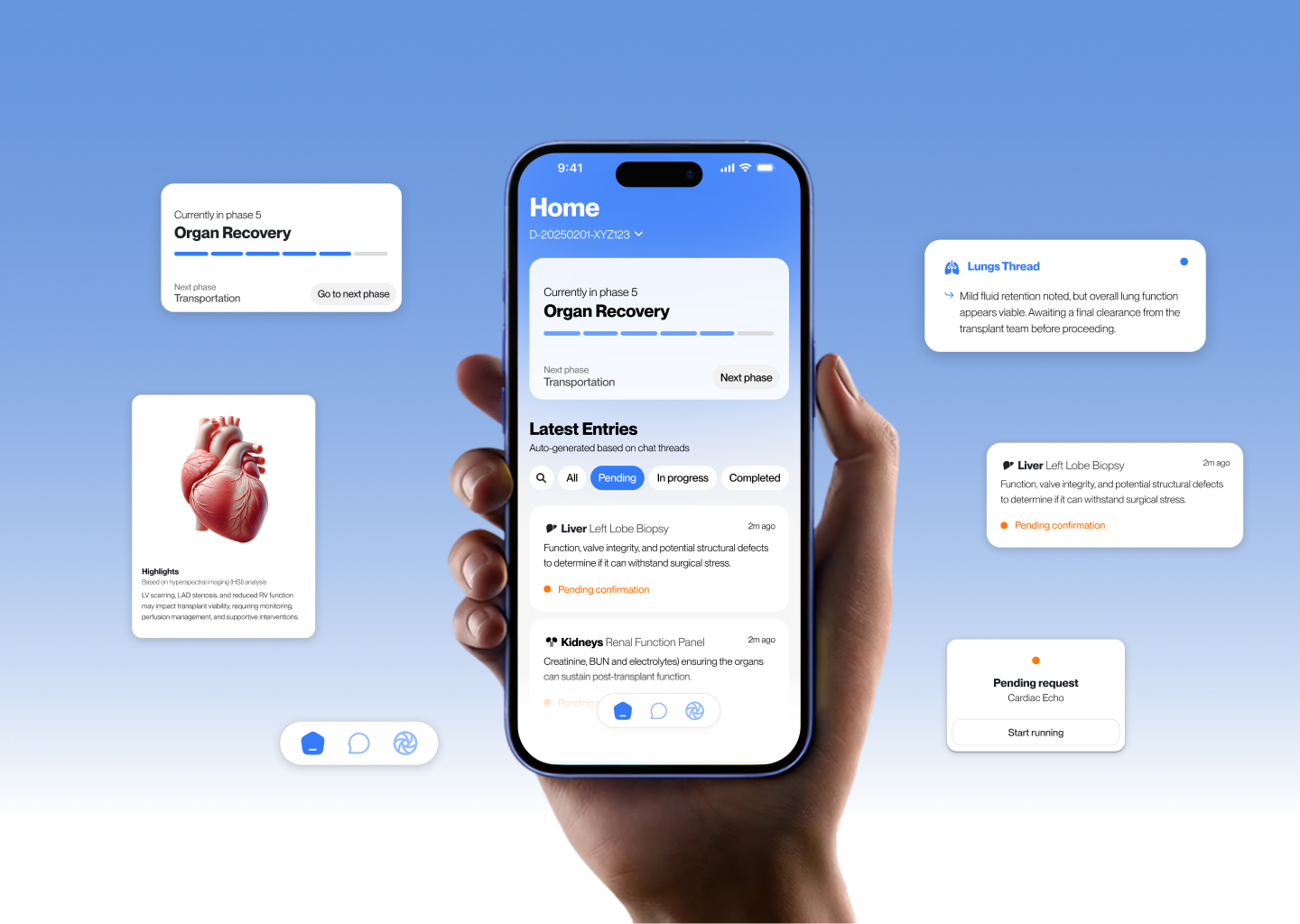
Final Screens
The final mobile interface delivers a fast, intuitive experience focused on urgent decision-making. Organ profiles, alerts, imaging, and communication are unified in one place, accessible on the devices teams already use daily.
Expected Outcomes
With Numa, we set out to not just reduce inefficiencies—but to reshape how teams make life-saving decisions under pressure. These outcomes reflect our core goal: increasing organ utilization by enhancing clarity, speed, and trust.
AI + Imaging Technology
Numa integrates advanced AI and medical imaging tools to reduce subjectivity, improve decision confidence, and accelerate organ placement. Each layer of the tech stack addresses a specific need within the transplant workflow.
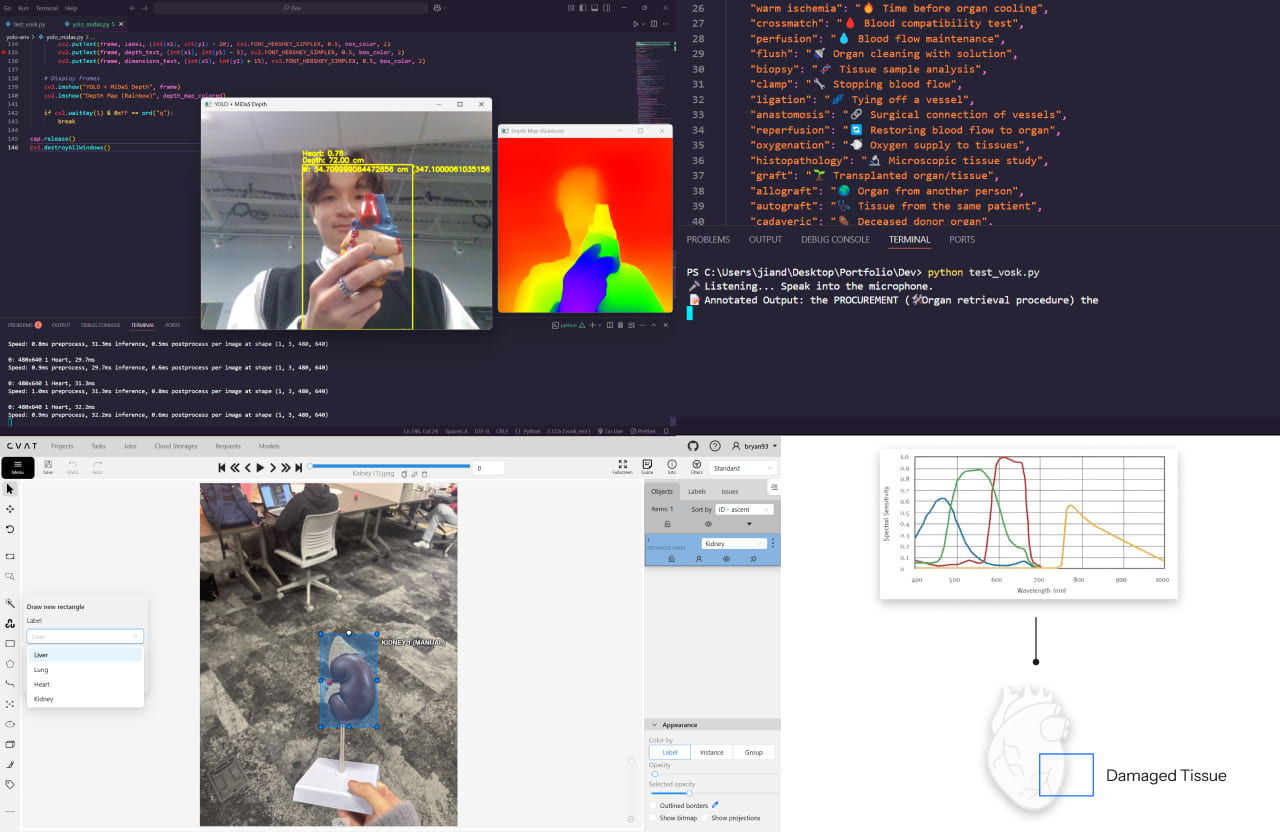
Hyperspectral Imaging (HSI)
Reveals biological data invisible to the human eye—oxygenation, tissue density, perfusion.
Outcome: Enables more confident decisions by identifying non-viable tissue early.
Stereoscopic Lens
Captures depth for accurate 3D organ reconstruction.
Outcome: Assists surgeons in evaluating shape, size, and compatibility before transport.
YOLOv8 + Intel MIDAS
Object detection + depth estimation from flat 2D images.
Outcome: Identifies organs automatically and helps prioritize high-viability candidates faster.
CVAT AI + VOSK
CVAT supports fast annotation and segmentation. VOSK transcribes spoken observations into structured medical notes.
Outcome: Reduces manual data entry and creates consistent logs during evaluations.
Why It Matters
In transplant logistics, clarity saves lives. Surgeons and coordinators must make high-stakes decisions within minutes, often with fragmented or outdated information. Without clear imaging and reliable data, viable organs are lost, and lives are left hanging in the balance.

“It’s very possible that some organs were rejected because transplant centers didn’t have enough data at their fingertips.”— Dr. Nicole Schockor
Stats at a Glance
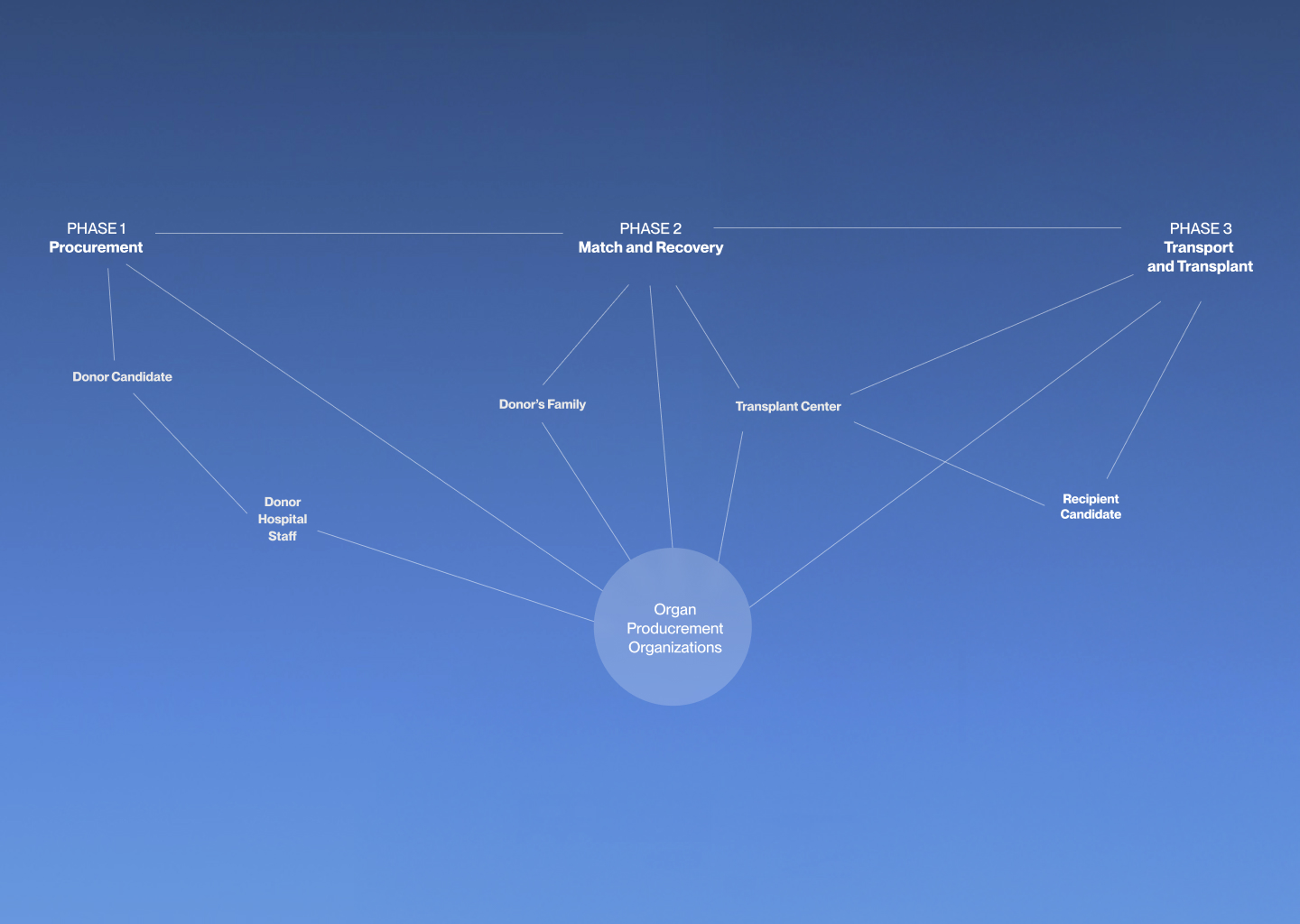
Organ Donation Process
The organ donation journey involves multiple organizations and stakeholders working together across seven tightly coordinated phases.
1. Identifying Potential Donor
Brain death is determined and confirmed to meet ethical and legal standards.
2. Notifying OPO
The hospital contacts the regional Organ Procurement Organization (OPO) to begin coordination.
3. Donor Assessment & Consent
OPO coordinator approaches the family and obtains consent to proceed with donation.
4. Matching Donor to Recipient
Donor data is entered into UNOS. Transplant surgeons review organ condition and patient needs.
5. Organ Recovery
Surgical staff recovers viable organs and prepares them for transport.
6. Transport of Organs
Organs are transported by ground or air depending on the recipient’s location.
7. Transplant Surgery
The transplant is performed at the recipient’s hospital by the assigned surgeon.
OPO Network Performance
Organ Procurement Organizations (OPOs) operate independently with varied performance across regions. Without a centralized platform or enforcement system, underperformance persists.
Where Organs Are Lost
There are seven main reasons why organs go to waste. Six of them occur while under OPO control—highlighting inefficiencies in communication, logistics, and follow-through.
Underlying Systemic Gaps
Our research revealed that inefficiencies in organ procurement weren’t caused by isolated failures. Instead, they stemmed from a lack of shared tools, fragmented workflows, and invisible handoffs across organizations. While each stakeholder fulfilled their responsibilities, no one had full visibility into the entire process.
Research & Synthesis
Our understanding deepened with each conversation.
We conducted 12 interviews with stakeholders across the OPO ecosystem—organ procurement professionals, transplant surgeons, medical staff, and policy advocates. These sessions yielded over 200+ insights and reframed our assumptions.
“The biggest delays weren’t from transport. They were from fragmented communication, inconsistent evaluations, and a lack of shared context.”
Themes (Phase by Phase)
- Fragmented Communication: Slow, siloed channels delayed life-saving decisions.
- Subjective Evaluations: Organ viability decisions varied due to inconsistent data formats and lack of visual standards.
- Transport Mishaps: Improper storage, routing errors, or cold ischemia time led to unnecessary discards.
- Cumbersome Communication & Documentation: Existing tools caused friction and manual work under pressure.
- Lack of Collaboration with Transplant Centers: OPOs and TCs often made decisions without shared insights.
- Responsibility to Donor Families: Staff emphasized the importance of honoring each donor's legacy.
- Cumbersome Communication: The need for real-time, in-platform messaging and updates.
- Lack of Collaboration with TCs: Visibility gaps delayed or derailed transplant decisions.
- Procurement Image Quality: Evaluation photos were often taken via smartphones with inconsistent results.
How Might We
Through each stage of the project, we continually reframed our design challenges based on user feedback and technical constraints:
- How might we create a seamless, real-time communication system between OPOs and transplant centers to ensure timely organ allocation and reduce organ discards?
- How might we ensure consistent and accurate information flow between OPOs and transplant coordinators to prevent delays and improve organ utilization?
- How can we streamline the data logging process for OPOs to reduce manual entry, minimize errors, and accelerate critical decision-making for organ allocation and transport?
Early Ideation & Crazy 8s
Before arriving at a cohesive product ecosystem, we explored bold, unconventional ideas through sketching exercises and Crazy 8s. These early concepts allowed us to think freely—prioritizing user needs over feasibility—and helped us break out of linear thinking.
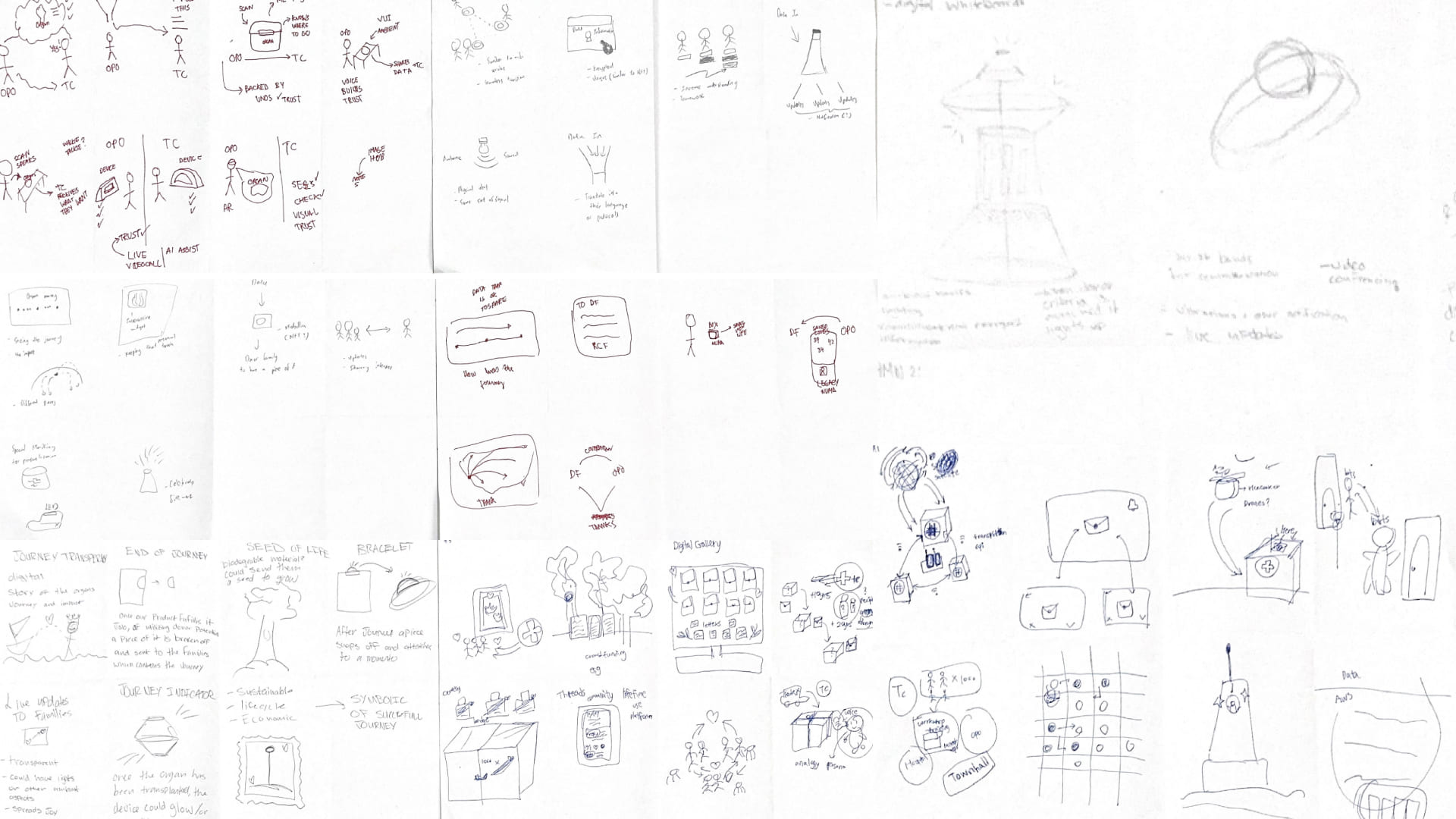
Blue Sky Concepts
Ideas ranged from digital twins and immersive organ visualizations to a slap-on tracker (like a slap band) and a smart scanning box designed to assess organs in the field.
What We Learned
Sketching surfaced pain points around information flow, environment constraints, and visibility. It also revealed opportunities to blend analog and digital tools—helping us shape the final modular ecosystem.
Product Refinement
After early ideation, we began refining the system architecture based on feasibility, stakeholder feedback, and the clinical realities of organ procurement. We grouped features into modules and evaluated them based on value, usability, and deployment complexity.
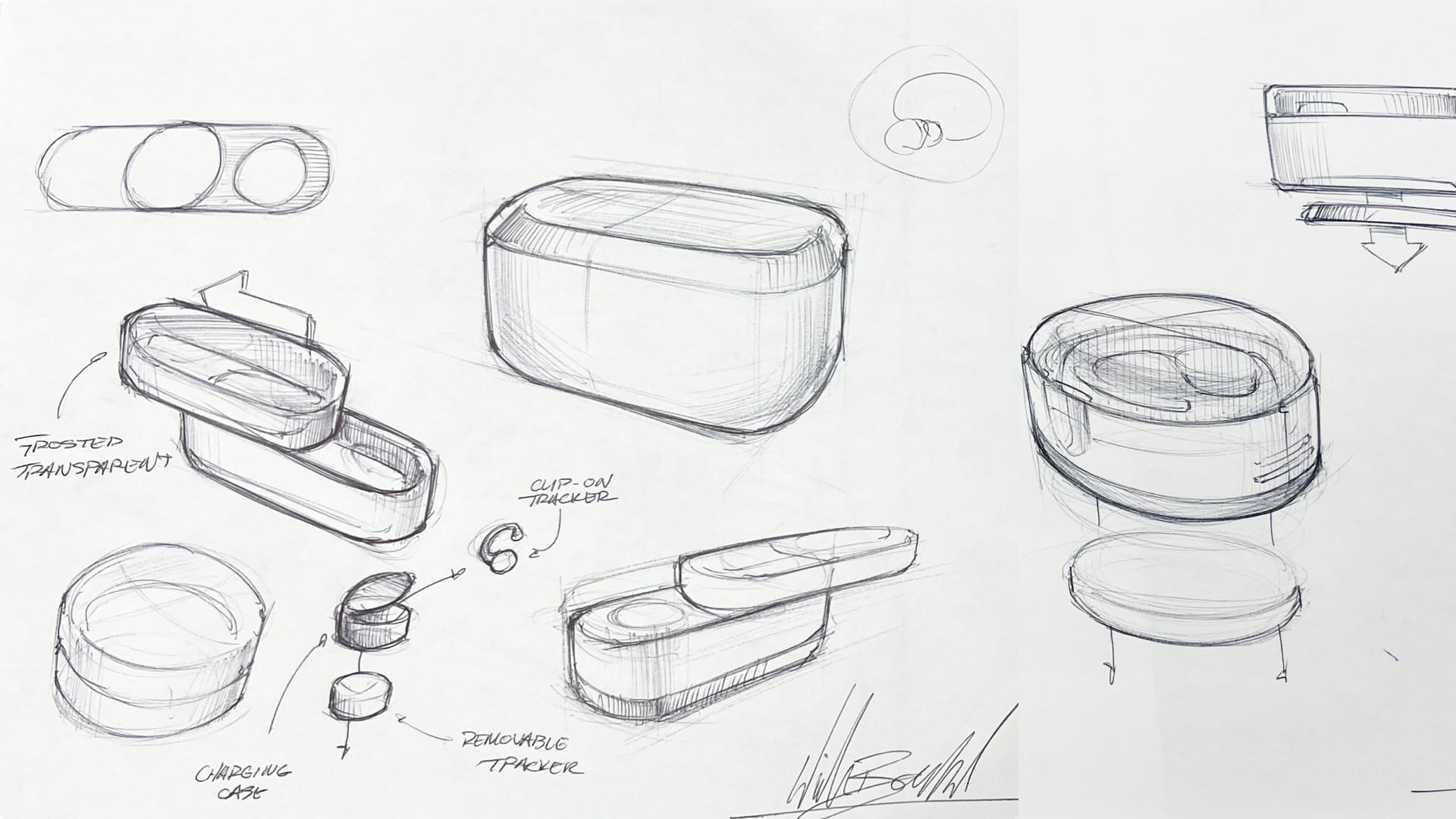
Modular Thinking
We split Numa into interoperable components: an image-capture device, a collaborative platform, and a lightweight communication tool. This structure allowed for flexible integration into different hospital systems and varying workflows.
Strategic Tradeoffs
Some ideas—like donor legacy capsules or autonomous drones—were set aside due to technical or ethical concerns. Others evolved into simpler, more deployable versions that still met core needs.
Numa v1 Ecosystem
Our initial concept imagined a multi-part system to solve coordination issues across the procurement journey.

These components worked together—but posed implementation challenges that led to our product pivot.
Pivot to Practicality: A Product Evolution

Phase 1 — Wearable to Standalone Camera
- Wearables were impractical in high-stress surgical settings.
- Tracking was already handled by FedEx or couriers.
- Airplane connectivity limited real-time uploads.

Phase 2 — Standalone to Phone Attachment
- Standalone cameras required extra training.
- Users already carried powerful tools: smartphones.
- Phone attachments enabled fast deployment, using built-in tech.

Phase 3 — Mobile-First Workflow Redesign
- Rebuilt interface for time-sensitive phone use.
- Prioritized quick access to visuals, notes, and chat.
- Enabled async data sync + real-time transplant center feedback.
Second Phase: Mobile-First Redesign
Following our product evolution, we entered Phase 2: a mobile-first redesign built around the realities of the field. This phase emphasized speed, familiarity, and clarity—all rooted in the insights we gained during earlier pivots.
- How might we leverage automation to reduce documentation?
- How might we create a standardized organ profile across platforms?
- How might we build trust and synergy between OPOs and transplant centers?
“If we had an easy, organized mobile interface, we could go through reviews faster and better.”— Dr. Nicole Schockor
Usability Testing
We conducted 7 usability tests with transplant professionals and OPO coordinators to validate the mobile workflow and camera attachment. Additionally, we partnered with UNOS Lab to test our platform with industry stakeholders, including Devin Holland, Business Development & Strategic Partnerships Lead.

Testing Highlights
- Surgeons and coordinators favored the phone-based solution for its familiarity and speed.
- Most participants preferred fewer logins and centralized alerts over multi-platform navigation.
UNOS Lab Feedback
- The platform aligns with clinical expectations and UNOS workflows.
- Participants valued the simplified UI during high-pressure situations.
- Data organization and camera quality stood out as key strengths.
Reflection
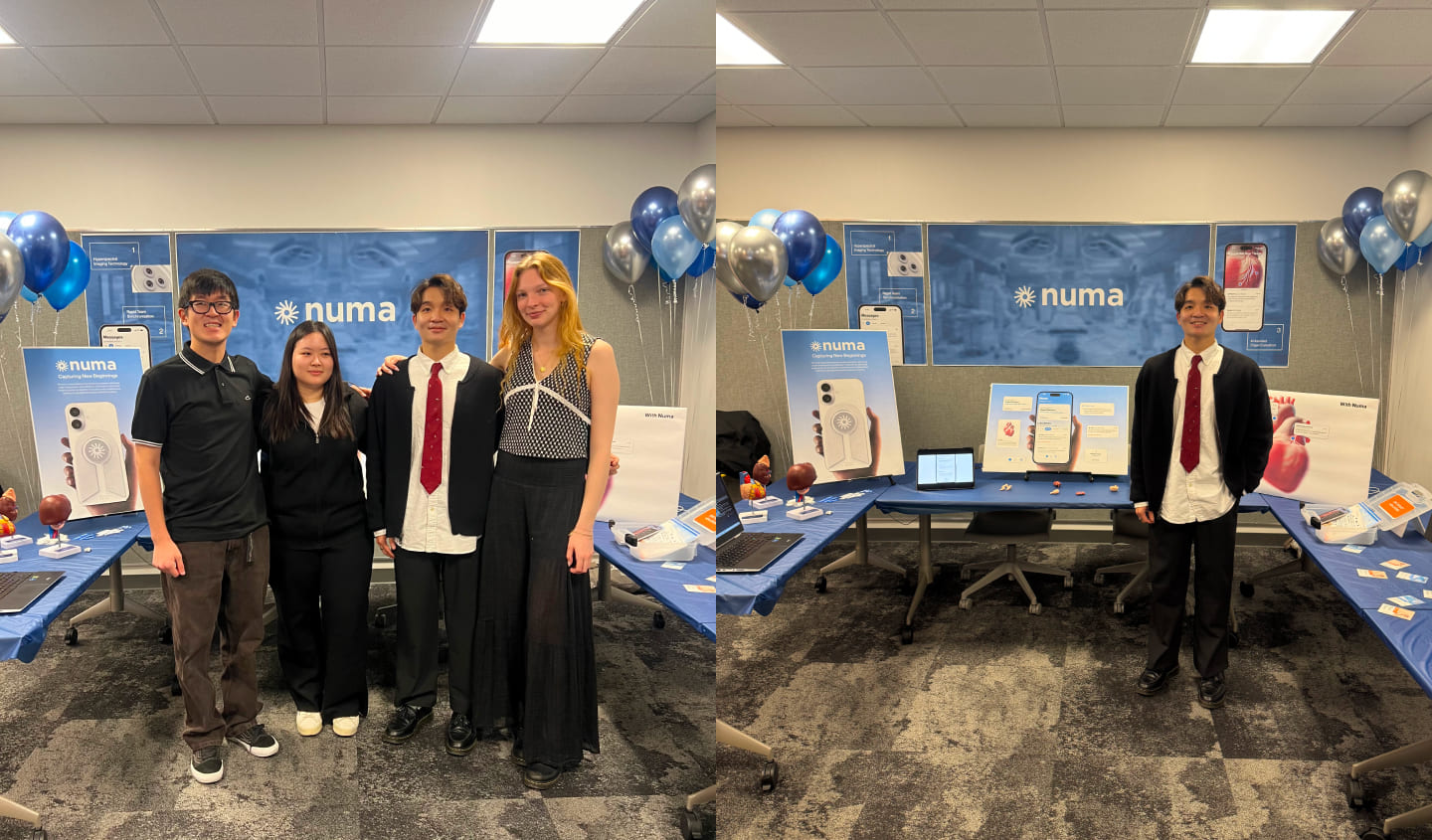
From day one, our mission was clear: increase organ utilization by solving real inefficiencies in the moments that matter most. What began as a technological exploration quickly became a deeper systems challenge. It required empathy, adaptability, and clarity.
Every design pivot, whether from wearable to mobile or hardware to ecosystem, was grounded in field reality. We didn’t just ask how it could work. We asked: will this work for them, here, now?
Numa is more than a product—it’s a shift in how we collaborate around life-saving decisions. It shows what happens when clarity, technology, and humanity meet at the exact point of need.
What’s Next?
References
Curious to explore more? Here’s where our research came from:
- organdonor.gov — U.S. government statistics and process overview for organ donation.
- organdonationreform.org — Reporting on underutilized organs, policy issues, and reform proposals.
- KFF Health News — Interviews with transplant surgeons and analysis of system inefficiencies.
- STAT News — Data on kidney discard rates and transplant decision-making.
- aopo.org — Association of Organ Procurement Organizations: performance reports, tier breakdowns.
- DaVita Newsroom — Commentary on innovation in procurement and OPO transparency.
- UNOS (United Network for Organ Sharing) — Central organ matching system and DonorNet platform documentation.